Do you feel overwhelmed and afraid that you might get sick?
It’s been a long winter, full of bugs and cost-of-living pressures, on top of the usual mix of work, education, health management and caregiving responsibilities.
Stress is an inevitable part of life. In the short term, our stress response has become a survival mechanism to help us be more alert in fight or flight situations.
But when stress is not treated, it weakens the immune system and makes us more vulnerable to diseases like the common cold, the flu, and COVID.
Stress makes it harder to fight germs
When the immune system begins to break down, the virus that would normally be under control begins to spread.
As soon as you start feeling sick, the stress response is heightened, making it harder for the immune system to fight the disease. You may get sick more often and for longer, without having enough immune cells organized and ready to fight back.
In the 1990s, American psychology professor Sheldon Cohen and his colleagues conducted a series of studies in which healthy people were exposed to upper respiratory infections, via airborne droplets. -hloko is inserted directly into their noses.
After that, these participants were isolated in the hotel and closely monitored to find out who was sick.
One of the most important predictors of who will get sick is chronic stress.
Cortisol suppresses the immune system
«Short-term stress» is stress that lasts minutes to hours, while «chronic stress» lasts for several hours a day for weeks or months.
When faced with a perceived threat, mental or physical, the hypothalamus area of the brain sounds the alarm. This means the release of many hormones, including adrenaline and cortisol.
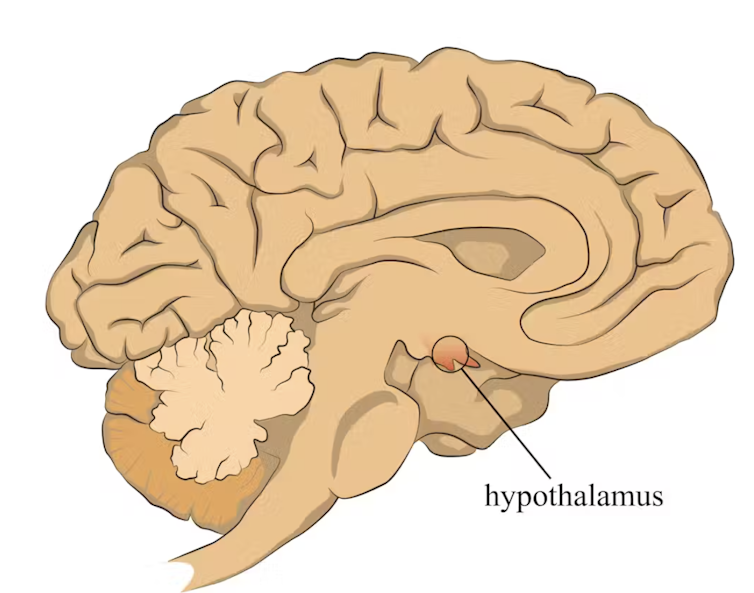
stefan3andrei/Shutterstock
In a normal stress response, cortisol levels increase rapidly when stress occurs, then quickly return to normal once the stress level is reduced. In the short term, cortisol suppresses inflammation, ensuring that the body has enough energy to respond to an immediate threat.
But over time, chronic stress can be dangerous. A Harvard University study from 2022 showed that people who experience stress leading up to their exposure to COVID are more likely to have long-term exposure to COVID. They described this suffering as stress, potential anxiety, depression, anxiety about COVID and loneliness.
Sufferers who were suffering had a 50% greater risk of long-term COVID compared to other participants. Cortisol has been shown to be higher in the most severe cases of COVID.
Stress causes inflammation
Inflammation is a temporary response to injury or infection. It is responsible for marketing your body’s own cells so that the right cells are in the right places at the right time and in the right conditions.
Immune cells also store the memory of that threat to respond more quickly and effectively in the future.
Initially, circulating immune cells recognize and migrate to the site of infection. Messenger proteins, known as pro-inflammatory cytokines, are released by immune cells to signal danger and help, and our immune system responds to reduce the threat.
During this response to infection, if the immune system produces too many of these chemicals, it can cause symptoms such as a runny nose and a runny nose.

Alyona Mandrik / Shutterstock
What about chronic stress?
Chronic stress causes high secretion of cortisol, which remains elevated even in the absence of immediate stress.
The immune system becomes depressed and does not respond to this stress of cortisol, increasing the «quiet» low-level inflammation and the production of pro-inflammatory cytokines (proteins messenger).
Immune cells become exhausted and begin to malfunction. The body loses the ability to reduce the inflammatory response.
Over time, the immune system changes the way it responds by reprogramming the «down-guard». The immune system loses the first opportunities to destroy threats, and the recovery process can take a long time.
So how can you manage stress?
We can strengthen our immune system and natural defenses by managing our stress levels. Instead of letting stress build up, try to address the problem early and often by:
1) Getting enough sleep
Getting enough sleep reduces cortisol levels and inflammation. During sleep, the immune system releases cytokines, which help fight infection and inflammation.
2) Exercise regularly
Exercise helps the lymphatic system (which transports body fluids as part of the immune system) to circulate and allows the body’s immune cells to scan for threats, while sweat flushes out toxins. Physical activity also lowers stress hormone levels through the release of positive brain signals.
3) Eating healthy food
Making sure that your diet contains enough nutrients – such as B vitamins, and a full range of minerals such as magnesium, iron and zinc – during times of stress has a positive effect on stress levels. common sense. Staying hydrated helps the body flush out toxins.
4) Socializing and practicing meditation or mindfulness
These activities increase endorphins and serotonin, which improve mood and have anti-inflammatory effects. Breathing exercises and meditation stimulate the parasympathetic nervous system, which calms our stress responses so we can «reset» and reduce cortisol levels.![]()
Sathana Dushyanthen, Academician & Lecturer in Cancer Sciences & Digital Health| Superstar of STEM| Scientist, University of Melbourne
This article is reprinted from The Conversation under a Creative Commons license.
#feel #overwhelmed #afraid #sick